In modern hepatology, the treatment of chronic hepatitis B (CHB) has achieved significant success due to the introduction of nucleoside/nucleotide analogues (NA). First-line drugs such as Tenofovir (TDF, TAF) and Entecavir have become the gold standard: they effectively block the reproduction of the virus, putting the disease in a controlled phase. However, clinical practice has revealed a serious limitation: suppressing the virus does not always mean restoring the liver.
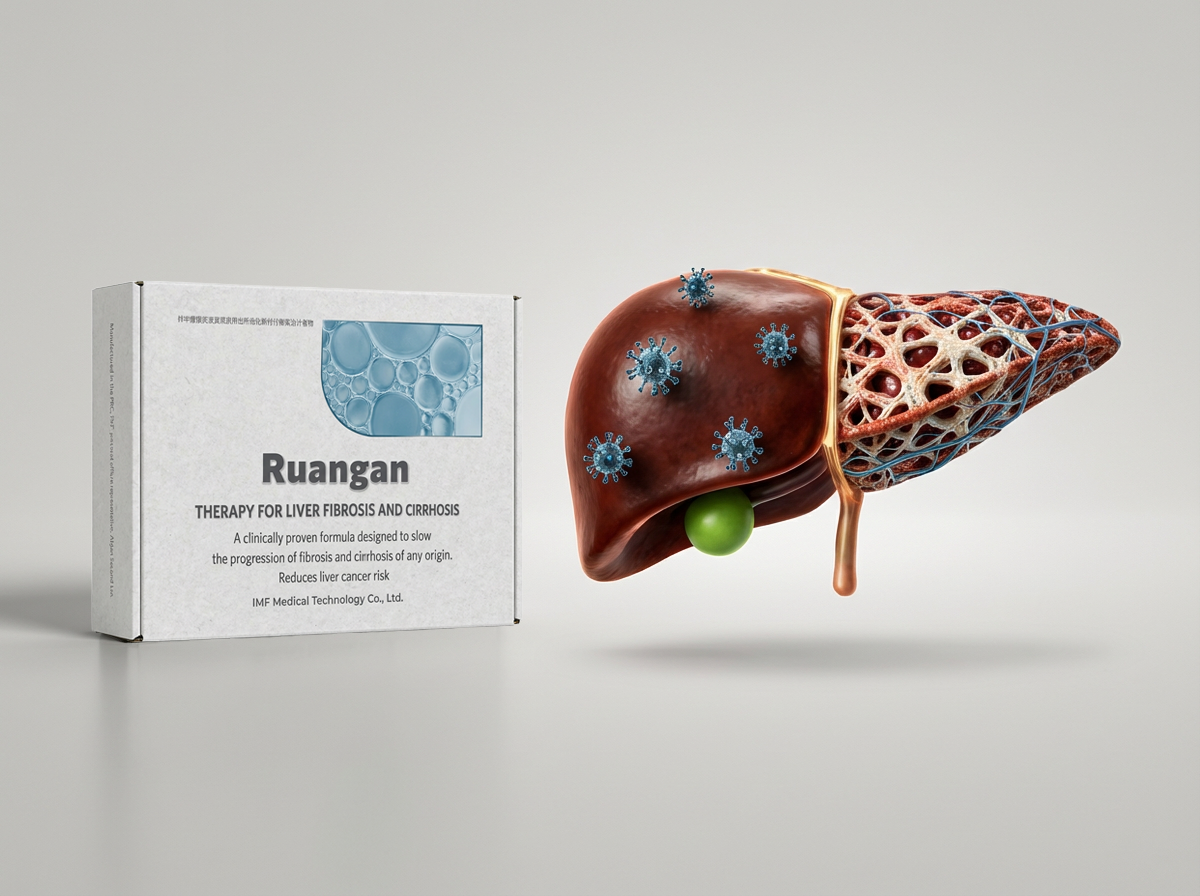
In a significant proportion of patients, despite the zero viral load, liver fibrosis regresses extremely slowly or remains stable, maintaining the risk of developing cirrhosis and carcinoma. In this context, the drug Fufang Bijia Ruangan Pian (Ruangan) is considered as a necessary element of therapy. But studies clearly indicate that this drug only reveals its therapeutic potential in conditions of suppressed viral activity.
Let’s consider the biochemical and clinical reasons why the combination of Tenofovir + Ruangan is considered the most promising treatment strategy today.
Viral activity and fibrogenesis: different mechanisms of pathology
To understand the logic of combination therapy, it is necessary to separate two parallel processes that destroy the liver:
- Viral replication and inflammation. The hepatitis B virus (HBV) is introduced into hepatocytes, using their resources to create copies of itself. The immune system attacks infected cells, causing them to die (necrosis) and become permanently inflamed.
- Structural adjustment (Fibrosis). In response to cell death, liver stellate cells (HSCs) are activated. They try to ‘patch up’ the damage by synthesizing collagen. In chronic inflammation, this process gets out of control, and the liver becomes overgrown with dense scar tissue.
The problem of Ruangan Monotherapy:
If only an antifibrotic drug (Ruangan) is used against the background of an active virus, the therapy will be ineffective. The rate of formation of new scars, stimulated by inflammation, will exceed the rate of their resorption by the drug. It is impossible to make ‘repairs’ while the’ house ‘is still on fire.
Tenofovir as a basic therapy: elimination of the etiological factor
Tenofovir (in particular, its modern form TAF — Tenofovir alafenamide) acts on the cause of the disease. Being a reverse transcriptase inhibitor, it blocks the mechanism of copying viral DNA.
Combined Tenofovir functions:
- Virological response: Rapid reduction of HBV DNA levels in the blood to undetectable levels.
- Relief of inflammation: Cessation of active liver cell death, which leads to normalization of ALT and AST levels.
- Creating conditions for regeneration: By eliminating the chronic damage factor, Tenofovir creates a ‘window of opportunity’ where recovery processes can prevail over destruction processes.
However, Tenofovir itself has little effect on already formed, mature fibrosis (stages F3–F4), since it does not have a direct fibrolytic effect.
Ruangan: pathogenetic restoration of tissue structure
When the viral load is suppressed by Tenofovir, Ruangan takes over. Its task is to eliminate the consequences of prolonged inflammation.
The mechanism of action of the drug in conditions of a ‘clean’ viral background becomes as effective as possible:
- Activation of matrix degradation: Ruangan stimulates the production of matrix metalloproteinases — MMP), enzymes that can break down dense type IV collagen fibers. In the absence of new inflammation (thanks to Tenofovir), this process leads to a real reduction in the volume of scar tissue.
- Inhibition of residual HSC activation: Even after the virus is removed, stellate cells can remain active by inertia. Ruangan blocks signaling pathways (TGF-β1/Smad), returning these cells to a dormant state or triggering their apoptosis.
- Improvement of microcirculation: Restoration of blood flow in the liver sinusoids improves the delivery of oxygen and drugs to hepatocytes, accelerating their regeneration.
Clinical efficacy of the combination: analysis of the evidence base
The advantage of co-administration of drugs is confirmed by large randomized trials.
The most significant study isNCT01965418, published in the Journal of Infectious Diseases. , which compared the effectiveness of Entecavir monotherapy (a class analog of Tenofovir) and the Entecavir + Ruangan combination in patients with severe fibrosis.
Results after 72 weeks of therapy:
- Fibrosis regression rate: In the combination therapy group, significant histological improvement was observed in 38.7% of patients, while in the monotherapy group-only in 23.9%.
- Cirrhosis reversal: In patients with initial cirrhosis of the liver, the combined scheme made it possible to remove this diagnosis (confirmed by biopsy) in 41.5% of cases.
The researchers concluded that the addition of Ruangan significantly enhances the antifibrotic effect of antiviral therapy, without increasing the frequency of side effects.
Therapy strategy: algorithm of actions
Based on research data, the current treatment protocol for patients with CHB and fibrosis is as follows::
- Initiation of antiviral therapy: Prescribing Tenofovir (or Entecavir) is a mandatory first step. The goal is to achieve aviremia (PCR of HBV DNA ‘not detected’).
- Enabling antifibrotic therapy: Ruangan is prescribed either simultaneously with the start of antiviral therapy (to prevent progression), or immediately after achieving a virological response.
- Course duration: Liver tissue remodeling is a slow process. The optimal duration of the combined course is from 48 to 72 weeks.
- Monitoring: Efficacy monitoring is performed every 6 months using non-invasive methods (elastography, biochemical fibrosis panels) and PCR diagnostics.
Conclusion
The combination ‘Tenofovir + Ruangan’ is a scientifically based approach to the treatment of chronic hepatitis B with fibrosis. This is an example of synergy, where each component solves its own problem: Tenofovir eliminates the cause (virus), and Ruangan eliminates the consequences (scar tissue). Only when used together can these drugs achieve the main goal — not just to stop the disease, but to restore the liver to its normal structure and function.
Sources:
Evidence-Based Complementary and Alternative Medicine
ClinicalTrials.gov
Frontiers in Pharmacology (2022)